IEEE Pulse – At the Interface of Disciplines
IEEE Pulse – At the Interface of Disciplines

Five years ago, Jeffrey Karp sat down to a dinner party with Massachusetts General Hospital dermatologist R. Rox Anderson. The two started talking, and by the end of the evening, Karp—himself a bioengineer at the nearby Brigham and Women’s Hospital—knew he wanted to make a collaboration happen between them. But on what? As he thought, he twisted his ring—his nickel allergy had flared up, and the skin on his finger was chafed and raw. Twist, and think; twist, think. And then it hit him: up to 45 million people in the United States shared his allergy, and the best measures they had to control it were small-molecule chelating creams with a dangerous tendency to leach into the skin.
That realization kicked off a three-year collaboration between the pair culminating in a 2011 Nature Nanotechnology publication that detailed the creation of a new, nanoparticle-based skin barrier cream 11 times more potent than existing versions and with none of the risk. The trick was in the size: the chemical compounds of calcium carbonate and calcium phosphate that Karp used bound naturally to nickel, but by shrinking them down to smaller than 500 nm, he’d hiked up the amount of surface area available to snatch up the nickel ions. And by the same token, by engineering the particles to all be larger than 70 nm—more than triple the size a particle would need to be to slip into the skin—he also ensured that they’d stay right on the surface of the flesh, where they should. Suspended in a simple glycerin emollient, the particles worked perfectly, capturing nickel ions before they could transfer to pig skin and lab mice, then washing harmlessly away. It was a simple solution with transformative potential—at least for allergy sufferers like himself.
NANO AND NATURE
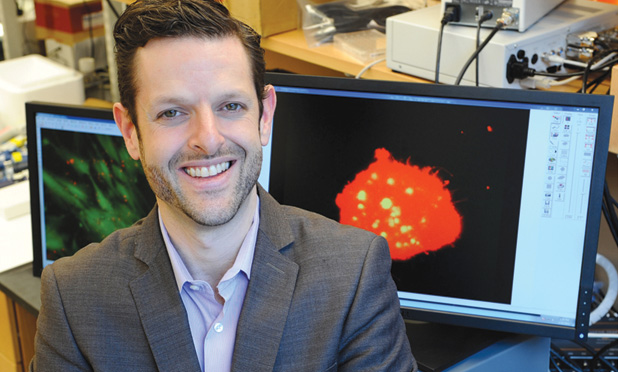
Karp is the codirector of regenerative therapeutics at Brigham and Women’s Hospital, Boston, Massachusetts. He works out of a chaotic office littered with books, papers, and at least two Canadian flags—tokens of his Ontario origins. His work runs the gamut from engineering better stem cell therapies, to inventing smarter biomaterials and diagnostic devices—anything, really, that will make the most difference in care in the least amount of time, and ideally with as many academic disciplines folded in as possible. “Innovation happens at the interface of disciplines,” he tells me, “and it means that you’re constantly learning new things, you’re never static—from a scientific perspective, the science is never boring.”
Karp’s nickel work with Anderson was arguably the most quintessentially nanotechnological of his projects to date, but it’s far from his only. Indeed, he first came to fame in early 2008, with the publication of a next-generation gecko-inspired adhesive bandage, developed by a team led by himself and his mentor, the Massachusetts Institute of Technology’s Robert Langer. Flexible, biodegradable, and perfect for internal tissues, the bandages were made from nanomolded polymers sculpted with a pattern of tiny pillars on one surface. The trick, of course, was in those pillars, which were scaled just nanometers across and apart so that they could mechanically lock onto tissues through capillary action and atomic Van der Waals force, mimicking the famously sticky toes of the gecko (Figure 1). Coated with a film of sugar-glue for good measure, the bandage was more than doubly as adhesive as traditional dressings and worked perfectly on rat stomach and pig intestine—troublesome tissue typically fastened with staples or stitches.
 FIGURE 1 Fantastically small nanopillars capture the same physical and atomic forces that make the gecko’s toes so sticky, creating ideal bandages for inside and out. (Photo courtesy of Jeffrey Karp.)
FIGURE 1 Fantastically small nanopillars capture the same physical and atomic forces that make the gecko’s toes so sticky, creating ideal bandages for inside and out. (Photo courtesy of Jeffrey Karp.)
That invention earned Karp a spot on Technology Review’s annual list of the world’s 35 top innovators under 35, plus another the next year on Popular Mechanics’ list of biotech breakthroughs. But for Karp, it was only the start.
Not long after the gecko-tape, Karp’s lab came out with another line of nanocreations: self-assembling gels that could trap a given drug in dense tangles of nanofiber and release on cue. Here, the team used ascorbylpalmitate gel with hydrophilic and hydrophobic domains that snapped into long fibers just 20–300-nm thick around drug molecules and could be injected all together into problem areas, like the joint of a rheumatoid arthritis sufferer. There, the gel did nothing—until the right enzyme came along, for example, an inflammatory enzyme associated with the arthritis. Then, the nearest fibers to the enzymes suddenly disassembled, dumping their drug just long enough to tamp down the impending inflammation before reorganizing back together.
“The concept is that you’ll have enzymes [released due to the spike in inflammation],” explains Karp. “And as soon as they pop up, the gel stops being dormant, releases drugs, has an immediate impact, and then the enzymes go away, and the remaining part of the gel is then stable.” That particular research work won the Young Investigator Category in 2011 at the annual meeting of the Society of Biomaterials.
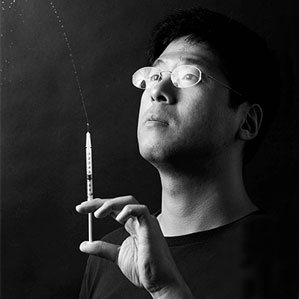
Just two years ago, Karp published on a third approach, this time using DNA—a natural nanoscale material—to reinvent on-the-spot cancer cell capture and diagnosis with a device inspired by the jellyfish. This time, he created multimicrons-long single strands of DNA coded to bind with leukemia cell surfaces, which he attached along the interior of a microfluidic chip etched in a herringbone pattern of channels. One end of the strand attached to the chip, the other was free floating in the channel ready to snatch up leukemia cells as they passed, like a jellyfish ensnaring its prey. So far, the device can pick up at least 60–80% of target cells, operating at ten times the speed of similar devices. “Evolution is the best problem solver,” Karp observes.
ENABLING THE FUTURE
“Nano is not something that we force,” Karp says of his inventions. “We focus on development, on finding medical problems that we’re interested, passionately, in solving.” Not everything he does requires nanotechnology, but much of it does, he explains, quite simply because it’s the key to enabling functionalities he might otherwise have been at a loss to design.
By and large, that functionality stems from the nanoscale’s inherently high surface area to volume ratio. Take the nickel allergy nanoparticles, for instance. They work so well because Karp was able to engineer the size of the particles to toe the line between safety—too large to slip into the skin—and efficacy—their massive surface area to volume ratio provided more opportunity to interact with the nickel ions.
It’s the same concept with the polymer drug-delivery fibers. “The nano component of it is really important,” Karp says. “And again it’s one of these high surface to volume phenomenon, where we want the gels to be responsive, and we want them to respond fast, so by incredibly increasing the potential surface area, we can maximize the response rate.” Same again with the jellyfish array, where just by using the nanowidth DNA strands instead of thicker wires, Karp was able to pack his microchip with a far denser, and therefore more efficient, network of cell-snaring “tentacles.”
“I look at nanotechnology very similar to how one might look at a microprocessor in a computer,” he says. “It’s there, you need it, and it’s one of these things that just keeps advancing at the speed of light. And if you don’t incorporate it into your work and harness it, then you’re going to be stuck in the Stone Age.”
Today, Karp is focused on extending those same projects—refining the jellyfish cell capture device to make it more efficient, and beginning to test patient samples. He’s also begun to experiment with applying his nanofiber drug-delivery fiber webs (Figure 2) to disorders like inflammatory bowel syndrome, and brain cancers like glioblastoma, where a drug-laden fiber tangle could fill the gap left by tumor removal, ready to release chemotherapeutics at the first sign of cancer-associated enzymes.
 FIGURE 2 Nanofibrous nets designed in Karp’s lab can lie dormant in problem areas, like an arthritic joint or a former tumor site, waiting for a chemical cue to pop open and flood the area with embedded drugs exactly when and where they’re needed most. (Photo courtesy of Jeffrey Karp.)
FIGURE 2 Nanofibrous nets designed in Karp’s lab can lie dormant in problem areas, like an arthritic joint or a former tumor site, waiting for a chemical cue to pop open and flood the area with embedded drugs exactly when and where they’re needed most. (Photo courtesy of Jeffrey Karp.)
And as for the nickel barrier cream? That, he admits, has already had its first human test. “I have tried it,” he admits. “It appears to work for me—although it’s not really a controlled study.” For everyone else, he expects that the cream should hit markets at the end of the year—and the gecko bandages will be hot on its heels, slated for 2015. Fast work, but that’s the Karp philosophy—making the most difference in minimal time.